AR in Healthcare: Boosting Surgical Precision by 12% in US Hospitals
Augmented Reality in healthcare is poised to significantly enhance surgical precision by 12% in US hospitals by 2025, integrating real-time data and visual overlays into surgical procedures for improved patient safety and operational efficiency.
The landscape of modern medicine is undergoing a profound transformation, driven by technological advancements that promise not just incremental improvements, but revolutionary leaps. Among these,
Augmented Reality in Healthcare: Improving Surgical Precision by 12% for US Hospitals in 2025
stands out as a particularly compelling and impactful development. This isn’t merely a futuristic concept; it’s a tangible reality that is already beginning to reshape how complex medical procedures are performed, offering unprecedented levels of accuracy and safety.
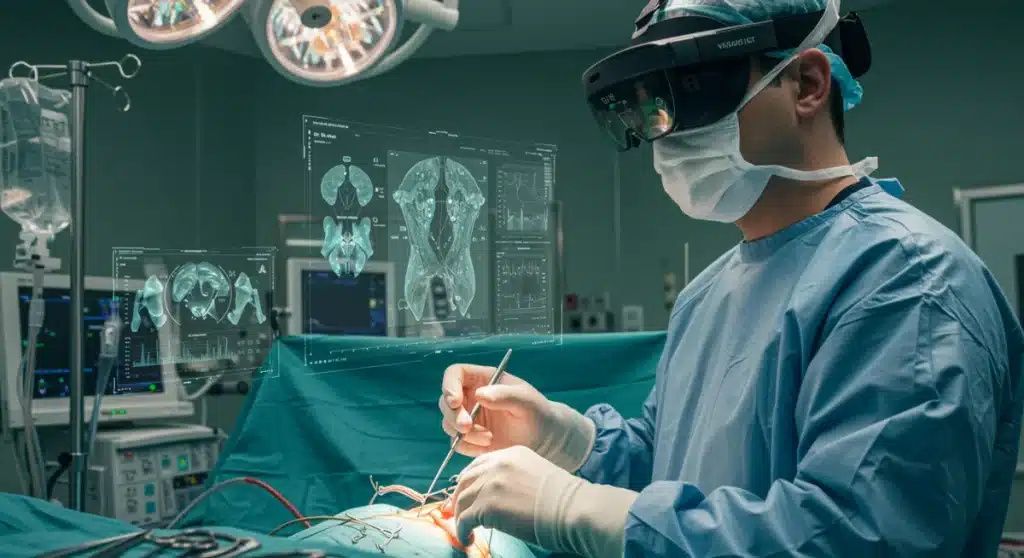
The Dawn of AR in the Operating Room
Augmented reality (AR) is rapidly moving from the realm of science fiction into the practical application within surgical suites across the United States. This technology overlays digital information onto a surgeon’s view of the real world, providing critical data in real-time without requiring them to divert their gaze from the patient.
This integration of virtual data with physical reality offers a new dimension of guidance during intricate procedures. Surgeons can visualize anatomical structures, pre-operative scans, and even vital signs directly on the patient’s body, creating a more informed and controlled environment.
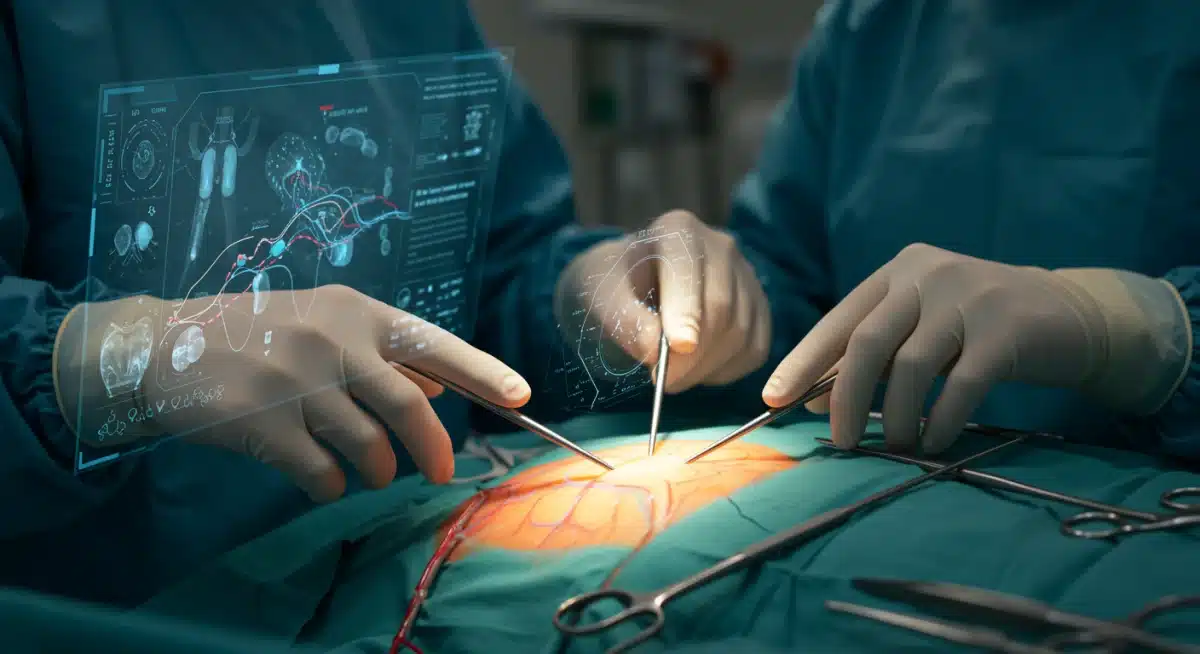
Enhanced Visualization and Navigation
One of the primary benefits of AR in surgery is its ability to enhance visualization. Surgeons can see through tissues, identify hidden blood vessels, or precisely locate tumors that might otherwise be difficult to ascertain with traditional methods. This capability is particularly crucial in minimally invasive surgeries where the field of view is often restricted.
- 3D modeling: AR systems can project detailed 3D models of organs and pathologies directly onto the surgical field.
- Real-time data overlay: Vital patient statistics, such as heart rate and oxygen levels, can be displayed without obstruction.
- Pre-operative planning integration: CT and MRI scans can be integrated and displayed dynamically during the procedure.
The ability to navigate complex anatomies with greater confidence translates directly into improved outcomes. Hospitals are increasingly investing in these systems, recognizing their potential to elevate the standard of care.
In conclusion, AR’s introduction into surgical settings marks a significant paradigm shift. By providing an augmented perspective, it empowers surgeons with more comprehensive information, leading to better decision-making and execution, thereby setting the stage for a new era of surgical precision.
Precision Boost: A 12% Improvement by 2025
The ambitious goal of improving surgical precision by 12% for US hospitals by 2025 is not an arbitrary figure; it’s a projection based on the demonstrable impact of augmented reality technologies. This improvement encompasses various aspects, from reducing incision sizes to minimizing collateral damage to healthy tissues.
Such a significant leap in precision has profound implications for patient recovery times, complication rates, and overall healthcare costs. The data compiled from early adopters of AR in surgery points towards a clear trend of enhanced accuracy and efficiency.
Surgeons using AR report a marked increase in their ability to perform delicate maneuvers with greater confidence. This is especially true in specialties like neurosurgery, orthopedic surgery, and interventional cardiology, where millimeter-level accuracy can be the difference between success and failure.
Minimizing Human Error
Human error, while inherent in any complex human endeavor, can have devastating consequences in surgery. AR acts as an intelligent co-pilot, providing continuous feedback and guidance that helps mitigate these risks. By presenting critical information directly within the surgeon’s field of view, it reduces the need for mental reconstruction of anatomy or constant glances at external monitors.
- Guided incisions: AR can project precise incision lines based on pre-operative planning.
- Tool tracking: Real-time tracking of surgical instruments ensures optimal positioning and trajectory.
- Reduced fatigue: By consolidating information, AR can lessen cognitive load and surgeon fatigue during long procedures.
The projected 12% improvement is an aggregate of these benefits, translating into tangible gains for both patients and healthcare providers. It signifies a future where surgical interventions are not only safer but also more effective, leading to better long-term health outcomes.
Ultimately, the drive for enhanced precision through AR is a testament to healthcare’s relentless pursuit of excellence. This technology is not just about doing things differently, but about doing them better, with a measurable impact on patient care.
Key Applications and Use Cases in Surgical Specialties
Augmented reality’s versatility allows for its application across a broad spectrum of surgical specialties, each benefiting from its unique capabilities. From complex neurological procedures to intricate orthopedic repairs, AR is proving to be a game-changer, tailoring its functionalities to meet specific clinical needs.
The technology’s ability to provide context-sensitive information makes it invaluable in situations where precision and real-time data are paramount. Its adoption is not uniform but is growing steadily as more evidence emerges of its efficacy and safety in diverse surgical environments.
Neurosurgery and Spinal Procedures
In neurosurgery, where margins of error are minuscule, AR offers unprecedented guidance. Surgeons can visualize tumor boundaries, critical neural pathways, and vascular structures with remarkable clarity, minimizing the risk of damage to surrounding healthy brain tissue.
- Tumor resection: AR assists in precisely defining tumor margins, ensuring complete removal while preserving healthy tissue.
- Spinal fusion: Provides real-time guidance for screw placement, reducing the risk of nerve damage.
- Biopsy guidance: Enables more accurate targeting for diagnostic biopsies in hard-to-reach areas.
Similarly, orthopedic surgeons leverage AR for precise alignment and placement of implants in joint replacement surgeries, leading to better functional outcomes and reduced revision rates. The technology ensures that components are positioned optimally, often exceeding the accuracy achievable with traditional methods.
The expanding array of AR applications underscores its potential to become an indispensable tool across the entire surgical landscape. Its adaptability to various procedures highlights its fundamental value in enhancing surgical performance and patient safety.
Technological Innovations Driving AR Adoption
The rapid integration of augmented reality into healthcare is not just a testament to its potential but also to the significant advancements in the underlying technologies. These innovations have made AR systems more powerful, user-friendly, and cost-effective, accelerating their adoption within US hospitals.
Improvements in hardware, software, and computational power have converged to create robust AR platforms capable of meeting the stringent demands of the operating room. The ongoing development in these areas promises even more sophisticated and seamless integrations in the near future.
Advanced Headsets and Software Platforms
Modern AR headsets are becoming lighter, more comfortable, and offer wider fields of view, making them practical for extended surgical use. Coupled with intuitive software interfaces, these devices can process and display complex medical imaging data in real-time.
- High-resolution displays: Provide crystal-clear overlays without obscuring the surgeon’s view of the real world.
- Gesture control: Allows surgeons to manipulate virtual objects and data without touching physical controls, maintaining sterility.
- AI integration: Artificial intelligence algorithms can analyze data and offer predictive insights or highlight potential risks.
The development of specialized AR software platforms for surgical planning and execution is also critical. These platforms integrate with existing hospital information systems, enabling seamless data flow and reducing setup times. They often include features for collaborative planning and remote assistance, further extending the utility of AR.
These technological strides are foundational to AR’s success in healthcare. Without these continuous innovations, the sophisticated level of surgical precision we anticipate would remain out of reach, underscoring the importance of ongoing research and development in this field.
Challenges and Considerations for Widespread Implementation
While the benefits of augmented reality in surgery are clear, its widespread implementation in US hospitals faces several challenges. These hurdles range from the technical complexities of integration to the financial investments required and the human factors involved in adopting new technologies.
Addressing these challenges systematically will be crucial for AR to reach its full potential and become a standard tool in every operating room. A multi-faceted approach involving technology developers, healthcare administrators, and medical professionals is essential.
Cost and Training Implications
The initial investment in AR hardware and software can be substantial, posing a barrier for some hospitals, especially smaller or rural facilities. Furthermore, integrating AR systems with existing hospital infrastructure requires significant IT resources and expertise.
- High upfront costs: Purchasing AR headsets and specialized software licenses can be expensive.
- Maintenance and upgrades: Ongoing costs for system maintenance, software updates, and technical support.
- Surgeon training: Extensive training is required for surgeons and support staff to proficiently use AR systems.
Beyond financial considerations, there’s the critical aspect of training. Surgeons and operating room staff need to be thoroughly trained not only on how to use the AR equipment but also on how to integrate it seamlessly into their existing workflows. This requires dedicated training programs and a commitment to continuous education.
Overcoming these challenges will require strategic planning, collaborative partnerships, and a clear demonstration of return on investment. Only then can AR truly transform surgical practices across all US hospitals, ensuring equitable access to its benefits.
Ethical Considerations and Patient Safety
The introduction of any new technology in healthcare, especially one as transformative as augmented reality in surgery, necessitates a thorough examination of its ethical implications and impact on patient safety. While AR promises enhanced precision, it also introduces new considerations that must be carefully managed to maintain trust and uphold medical standards.
Ensuring patient well-being remains the paramount concern. Therefore, robust regulatory frameworks, rigorous testing, and transparent communication are essential as AR becomes more prevalent in surgical settings.
Data Privacy and System Reliability
AR systems process and display sensitive patient data, raising critical questions about data privacy and security. Protecting this information from unauthorized access and cyber threats is non-negotiable. Hospitals must implement stringent cybersecurity measures to safeguard patient confidentiality.
- Data security: Ensuring that patient data displayed or processed by AR systems is encrypted and protected.
- System accuracy: Rigorous validation of AR system accuracy to prevent misinterpretation of anatomical data.
- Emergency protocols: Clear procedures for system malfunctions or technical failures during surgery.
Moreover, the reliability of AR systems is crucial. Any malfunction or inaccuracy during a procedure could have severe consequences. Continuous testing, redundant systems, and clear emergency protocols are necessary to ensure that AR enhances safety rather than introducing new risks. The ethical responsibility extends to ensuring that patients are fully informed about the use of AR in their procedures and provide informed consent.
Addressing these ethical and safety considerations proactively is vital for the successful and responsible integration of AR into surgical practice. By prioritizing patient trust and safety, healthcare providers can harness the full potential of this innovative technology while mitigating potential downsides.
The Future Outlook: Beyond 2025
The projection of a 12% improvement in surgical precision by 2025 is just a stepping stone in the broader journey of augmented reality in healthcare. Looking beyond this immediate milestone, the future promises an even more integrated and sophisticated role for AR, continually pushing the boundaries of what’s possible in surgical interventions.
As the technology matures, we can anticipate AR becoming an indispensable part of every operating room, evolving from a specialized tool to a standard component of surgical practice. This evolution will be driven by ongoing research, development, and a deeper understanding of human-computer interaction in clinical settings.
Integration with AI and Robotics
The synergy between augmented reality, artificial intelligence (AI), and robotics is set to unlock new levels of surgical capability. AI can process vast amounts of medical data to provide predictive analytics and real-time decision support, which AR can then visualize directly for the surgeon.
- AI-driven insights: Real-time AI analysis of patient data and surgical progress, displayed via AR.
- Robotics collaboration: AR guiding robotic arms for superhuman precision and stability in delicate procedures.
- Personalized medicine: AR systems tailored to individual patient anatomies and surgical plans.
Robotic surgery, already a field of high precision, will be further enhanced by AR overlays, allowing surgeons to control robotic instruments with even greater accuracy and a more intuitive understanding of the surgical field. This convergence of technologies will enable procedures that are currently considered impossible.
The journey of AR in healthcare is dynamic and continually evolving. The advancements beyond 2025 will likely involve increasingly intelligent, autonomous, and seamlessly integrated systems that not only assist surgeons but also actively enhance their cognitive and motor capabilities, leading to an unprecedented era of medical precision and patient care.
| Key Point | Brief Description |
|---|---|
| Surgical Precision Boost | Augmented Reality is projected to enhance surgical precision by 12% in US hospitals by 2025, improving patient outcomes. |
| Enhanced Visualization | AR overlays critical digital information directly onto the patient’s anatomy, providing real-time guidance. |
| Key Applications | Widely applicable in neurosurgery, orthopedics, and other specialties for superior accuracy and reduced error. |
| Future Integration | Beyond 2025, AR will integrate with AI and robotics for even greater surgical capabilities and personalized medicine. |
Frequently Asked Questions About AR in Healthcare
Augmented Reality in surgical procedures involves overlaying digital information, such as 3D anatomical models or real-time patient data, directly onto a surgeon’s view of the physical operating field. This enhances visualization and provides crucial guidance without diverting the surgeon’s attention from the patient.
AR improves surgical precision by offering enhanced visualization, precise navigation, and real-time data integration. It helps surgeons identify critical structures, guides instrument placement, and minimizes human error, leading to more accurate incisions and reduced collateral damage to healthy tissues.
While beneficial across many fields, specialties like neurosurgery, orthopedic surgery, and spinal procedures show significant gains. These areas often require extreme precision, where AR’s ability to provide detailed anatomical overlays and real-time guidance is particularly impactful for complex maneuvers.
Key challenges include the high upfront cost of AR hardware and software, the complexity of integrating these systems with existing hospital infrastructure, and the necessity for extensive training for surgical teams. Additionally, ensuring data privacy and system reliability are critical concerns.
Beyond 2025, AR is expected to become an integral part of surgical practice, evolving through deeper integration with AI and robotics. This synergy will enable even greater precision, personalized surgical approaches, and the capability to perform highly complex procedures with enhanced safety and efficacy.
Conclusion
The integration of augmented reality into healthcare, particularly its role in improving surgical precision, represents a pivotal moment in medical innovation. With a projected 12% enhancement in precision for US hospitals by 2025, AR is not merely an incremental upgrade but a transformative technology that promises to redefine patient care and surgical outcomes. While challenges related to cost, training, and ethical considerations remain, the demonstrable benefits in visualization, navigation, and error reduction underscore its immense potential. As AR continues to evolve and converge with AI and robotics, its impact will undoubtedly grow, ushering in an era of unprecedented surgical accuracy and personalized medicine, ultimately leading to healthier, safer futures for patients across the nation. The journey of AR in the operating room is just beginning, and its trajectory points towards a future where precision is paramount and possibilities are limitless.





